CHAPTER 1YOUR PROSTATE: A USER'S GUIDE
Let's be honest: The relationship between a man and his reproductive system is probably the most important one in his life. And as with every relationship that matters, we tend to take it for granted.
When everything works just right, men get to enjoy some of life's greatest pleasures: attraction, sex, desire, the making of children. And when everything is working right, why try to understand how it all operates? That would take all the romance out of it.
At a certain point, however, it becomes important for a man and his reproductive system to get acquainted in a whole new way. This time comes right around midlife—the point at which things can start to go wrong "down there." For a substantial proportion of men, sexual function or libido might decline. Urinary difficulties might start to show up. Or a routine physical might lead to a diagnosis of prostate problems: enlargement of the prostate gland, a urinary tract infection, a questionable result from the blood test used to detect prostate cancer (the PSA screening test), or even prostate cancer.
Many men have never really thought about the fact that their bodies contain prostate glands until they receive a diagnosis of prostate disease. Few men know much about where this gland is or what it does until it starts to malfunction (or, as is often the case, until cancerous cells are detected long before any malfunctioning becomes evident—which can seem like an ambush to a man who feels great one moment and becomes a cancer patient the next). But a lot of men are getting this wake-up call.
In the late 1980s, urologists began to use the PSA blood test to detect prostate cancer. Since that time, diagnoses have become far more common. Overall, the rate of prostate cancer diagnosis has risen by 67 percent since the middle of the 20th century. Today, 18 percent of men can expect to get a diagnosis of prostate cancer at some point in their lives. And just under 20 percent of men ages 55 to 74 develop some clinical signs of benign prostate enlargement.
Rates of prostate cancer are rising in part because of earlier detection and in part because the population is aging—prostate cancer is primarily a disease of older men. However, because of routine screening with the PSA test, we are now detecting this cancer in men in their forties and fifties. Getting to know your prostate couldn't hurt, because chances are good that you're going to end up addressing one or another prostate issue in your lifetime.
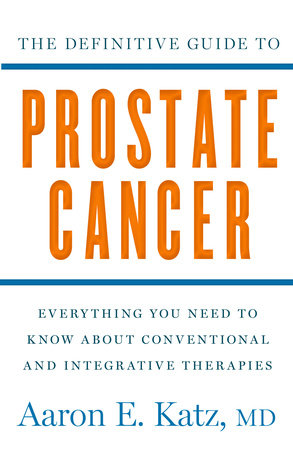
It's Okay to Be Scared . . .My best guess is that there's only one reason you have this book in your hands: You or someone you love has been diagnosed with prostate cancer or is at an especially high risk of developing the disease. Taking this step to inform yourself is commendable, especially if you're doing so in the days or weeks just after receiving a cancer diagnosis. This period of time can certainly be an emotional roller coaster.
If you are feeling traumatized and wish you weren't, or think that if you were truly manly, you wouldn't be feeling fearful or sad, you should know that these feelings are significant and in no way inconsequential. There's research to prove this: In one Harvard Medical School study of 350,000 men diagnosed with prostate cancer between 1979 and 2004, rates of suicide and death from heart attack and stroke—both of which can be linked to psychological stress—jumped during the first months following diagnosis.
The good news here is that this spike in death rates in the months following diagnosis stopped after 1993, when early detection efforts began in earnest. When the prognosis is good—as it is when prostate cancer is diagnosed in its earliest stages—the trauma is much less severe than when the cancer is diagnosed after it has spread too far to be curable. When the issues you face have more to do with making treatment choices in the interest of healing than with having to acknowledge a grim prognosis, psychological health isn't likely to crash and burn. You know you can do a lot to help yourself.
One reason for the enormous stress that used to accompany a prostate cancer diagnosis was the level of risk most treatments entailed—treatments that could be devastating to that all-important relationship between a man and his reproductive system. When I was a medical resident in the early 1990s, about half of men who underwent treatment for prostate cancer ended up impotent. Half ended up with urinary incontinence. The significant risks of impotence and/or incontinence made treatment choices close to impossible to make for some men.
Over the past 2 decades, death rates from prostate cancer have fallen, and treatments are now head and shoulders above what they once were, in terms of both effectiveness and reduced risk of side effects. Our rates of survival and cure from this disease are the highest ever, and in the last decade we have made many great advances in our understanding of the biology of prostate cancer cells, which has led us to vastly improved treatments.
Most important, we are learning that many men diagnosed with prostate cancer using modern early detection techniques do not need immediate treatment. A proportion of these men may never need treatment at all. That is why I believe this book is so needed: Men and their loved ones need to know that they can make an educated choice to postpone treatment, and they need a measured and up-to-date perspective on how to make this choice for themselves. In addition, they need to know that "watch and wait" can become a much more empowered process of "watch, wait, and act" when the holistic strategies described in this book are employed.
If you're not familiar with the idea of holistic therapies, you might imagine that they're about as valid as voodoo, astrology, alien abduction, or psychokinetics. But the reality is that herbal medicine, diet, and other "alternative" therapies are now converging with mainstream science-based, evidence-based medicine. One of the places where this is happening is my Center for Holistic Urology. In this book, I will not recommend any holistic therapy that does not have a solid basis in scientific validity and peer-reviewed research studies—for the most part, the same kinds of studies done on the drugs approved by the FDA and prescribed by doctors every day.
My primary aim in this book is to provide you with all the information you need following a diagnosis of prostate cancer, even if you are living with the disease and ongoing tests show that the cancer may have come back after treatment. To put all of this information to good use, you'll need to make a deeper, more detailed acquaintance with your prostate gland and with some other parts that reside in the same general neighborhood in the male body.
Your Prostate: An OverviewThe prostate gland is actually an integral part of the reproductive system. Situated underneath the bladder, wrapped around the urethra (the tube that carries both urine and semen out of the body), and nestled up against the front side of the rectum, the prostate is a gland made up of multiple lobes and encased in a membrane. The section of the urethra that passes through the prostate is the prostatic urethra.
A healthy young man's prostate weighs in at just over 3/4 ounce and is roughly the size of a large walnut or a small plum. During the buildup to ejaculation, the prostate secretes liquid through small pores that lie between it and the prostatic urethra. This liquid nourishes and carries sperm as they pass through the urethra on their voyage out.
On either side of the prostate sit seminal vesicles, which are small, pouchlike glands that contribute secretions to semen. Next to the seminal vesicles are Cowper's glands, which produce fluids that lubricate the urethra. Right at the confluence of these vesicles with the top of the prostate gland, two delicate vas deferentia (translation: vessels that carry away) also enter the urethra. Each of the vas deferentia extends from one of the testicles and up and around the bladder to get where they need to go.
The testicles, of course, are where sperm are produced. Immature sperm convene in the epididymis on top of each testicle. They mature there and wait for their big chance—the next ejaculation—at which point the vas deferentia contract rhythmically and draw sperm out to their date with destiny. Testicles also produce testosterone, the hormone that gives men sexual drive and the ability to have an erection. Testosterone also causes the growth of the prostate gland. One of the ways we can cause cancer to regress is to remove the ability of the testicles to produce this hormone. Today, we can do this surgically or with medications.
You may recognize the word root vas as the same one that initiates that dreaded word vasectomy—a procedure that severs or closes off these tubes to prevent sperm from leaving the body. It's interesting to note that some studies have found a link between vasectomy and prostate cancer. If you've already been through this procedure, you probably can't blame your prostate problems on it. Today, most evidence fails to support any connection between vasectomy and prostate cancer.
Copyright © 2011 by Aaron E. Katz, MD. All rights reserved. No part of this excerpt may be reproduced or reprinted without permission in writing from the publisher.