one
"Gradually and Then Suddenly"
In the fall of 1997, after I graduated from college, I began experiencing what I called "electric shocks"-stabbing sensations that flickered over my legs and arms every morning, as if I were being stung by tiny bees. The shocks were so extreme that as I walked to work from my East Village basement apartment, I often had to stop and rub my legs against a parking meter; if I didn't, my muscles would twitch and my legs would jerk. My doctor couldn't figure out what was wrong-dry skin, he proposed-and eventually the shocks went away. A year later, they returned for a few months, only to go away again just when I felt I couldn't bear them any longer.
In my twenties, the shocks and other strange symptoms-bouts of vertigo, fatigue, joint pain, memory problems, night sweats, tremors-came and went. For a year, every night around two a.m., I would wake up in a sweat to find hives covering my legs, leaving me itchy and wide awake, my pajamas and sheets so wet I had to change them. Doctors prescribed a daily dose of antihistamines until the hives went away. There was a test that suggested lupus, and then a follow-up that showed nothing was wrong; my lab work looked fine. "The tests were all negative. It's just one of those things that will go away," a specialist told me. I remember thinking, Don't you want to know why I have severe hives?
In the way of women who have internalized disordered ideas about food and control, I associated my strange bouts of fatigue and discomfort with eating poorly (even though I ate a reasonably healthy diet). It was easy, in those years, to feel that a lack of dietary discipline played a role in my exhaustion, because I could tell, vaguely, that certain foods made me feel worse, leading me to assume responsibility for my own unwellness. I toggled between the conviction that something had to be wrong-I didn't feel OK-and the conviction that I was to blame, and if I just stopped eating sugar, or pizza, say, I'd be fine.
One night, I woke up suddenly from a nightmare that a man in a dirty gray sweatshirt was stabbing me. My period had started, but in addition to the cramps I had a sharp pain in my lower right abdomen. The pain grew in magnitude until, heat flushing my body, I suddenly vomited. I thought perhaps I had appendicitis, but the pain went away an hour later, just as I was preparing to go to the ER. "Everyone feels cramps," my gynecologist told me when I asked about it.
At the advice of a friend, I went to see her gynecologist. This doctor listened and nodded when I mentioned the stabbing pain; I felt relief at the recognition. She did an exam and ultrasound. "I think you might have endometriosis, an immune-modulated disease where tissue from the uterus gets out and coats the abdomen and other organs, causing pain," she said. "But it doesn't really matter unless you want to get pregnant: it can cause infertility. Later we might want to address it with surgery. For now, I'd just take ibuprofen during your period." She gave me some tissues and I wiped myself, dressed, and left, puzzled by the way my pain had been relegated to a sign that my fertility might be compromised, not a problem in its own right.
When I was twenty-four, I started waking up with a feeling that a foggy miasma filled my brain. I would go for long runs before work to clear my head, lacing up my shoes, sweating off the sleep hangover. I thought everyone felt this way, that I was just fighting off a cold. But why was I so often on the verge of a cold-more than anyone else I knew? Periodically, I would start digging a little. In 2005, around the time of my twenty-ninth birthday, I was strangely enervated. I remember googling my symptoms and being struck by how much they matched those of several autoimmune diseases. I showed the results page to Jim; as the screen cast a blue light against his face, he nodded. "You are tired a lot for someone so young," he said. But then my doctors would reassure me that my lab work looked fine, and I'd return to trying to power through.
My tendency to ignore my symptoms derived in part from the fact that I grew up in a family that was largely indifferent to matters of health. As a child in Brooklyn-my parents were teachers at the school I attended-I had been raised not to think too much about my body. My parents had moved to the city from New Jersey, where they had grown up in large Irish American Catholic families. They were pragmatic and rather stoical. Like many in their baby boomer generation, they saw doctors as unquestionable experts. You didn't go to them unless you had a high fever or a bad fall or a wound that needed stitching. In that case, you got a diagnosis, you took medicine or had surgery, and you got better, more or less in that order. But if the doctor told you nothing was wrong, nothing was wrong. My parents believed in the power of Western medicine, and therefore so did I.
Ours was a family where health was not ever thought of as something to optimize or even talk about. So they took us to the doctor regularly and handed out Tylenol for fevers, but if the problem at hand was vague or seemingly minor, they tended to ignore it, telling us to buck up. As a kid, I had lots of "small things" wrong-bad allergies, muscle pain, poor digestion-which in retrospect I suspect were subtle clues about what was coming, but my parents did not pay much mind to them. I got used to being uncomfortable, in other words, and I internalized the idea that my mentioning my discomfort made me fussy-"The princess and the pea," my mother once said, in irritation, making it clear that I was demanding too much when I complained.
Still, there were moments that suggested something was not right. In July 2008, I had an early dinner with my mother-who was then on her fourth round of chemotherapy for stage 4 colorectal cancer-and my father on their patio in Connecticut. It was ninety degrees, and the sun was still up. The patio smelled of mint and basil and the air was thickly humid. I was shivering so much I put on a sweater. "You look more uncomfortable than I do," said my mother, giving me a sharp glance, her dark eyes tightening with unusual concern. "Are you OK?" I wasn't sure. When I woke up the next morning, I was exhausted and foggy headed. My mother knocked on the door, wanting to take a walk on the beach. Her black eyes were bright with the eagerness to live, and I found myself thinking that it seemed like my mother, despite undergoing chemotherapy, had more energy than I did.
All this was the backstory (not yet recognized as a story) to that moment in Vietnam when I found myself gazing at the angry red bumps on my wrist. This rash means something, I thought, trying to return to my book, as the wind whipped the palm trees and a large leaf clattered to the ground. All these little problems-they mean something. I stroked the bumps as if they could spell out a word that would unlock the mystery.
At home in Brooklyn, three days after Jim and I returned from Vietnam, I developed a low fever. It was February 2012. Inside our prewar apartment the radiators hissed and clanked, sending heat through the rooms. Jim had to travel to a conference. I slept strange hours tangled in sweaty sheets. My limbs felt heavy, watery. For two more weeks, I drifted along in a flu-like malaise that I thought was protracted jet lag. At the time, to support my life as a writer and journalist, I taught in the graduate creative writing program at New York University. I had also taken a job as a visiting writer at Princeton. I was trying to start writing a new book, but it was going slowly. I couldn't seem to focus.
The jet lag did not go away.
Teaching, which I had once loved, now felt onerous. In my Monday afternoon seminar, I had trouble forming sentences. As I spoke, with my students' faces turned earnestly toward me, I felt the point of my sentences receding further and further away. I slipped out on a break for a double espresso, but the caffeine failed to clear the wooliness in my mind. I got headaches and felt dizzy when I ate; my throat was often sore. I kept reversing phrases-saying things like, "I'll meet you at the cooler water."
One morning in March, I sat down at my desk in my sunny yellow study, only to start nodding off. My body felt like a vow that had been irrevocably broken.
I wondered whether my symptoms were just the result of too much aimless internet surfing-dog videos, flash sales-and a general lack of willpower. I wondered whether I was depressed; I had experienced a mild bout of depression in college, but this was nothing like that. Open as I was to the idea, I didn't believe that I was suffering from any kind of mental illness, nor did my symptoms or recent life events seem suggestive of one. My life had come together after the challenging few years following my mother's death. I had just published a memoir about her, a book I was proud of, because I felt it might help others who had suffered with feeling (as I had) that their grief was too large, too unseemly. I had been accepted into a writing residency for that summer and was excited to embark on my next book project. During my mother's illness, Jim and I had gotten divorced, our relationship strained by the devastation I felt. But now we had gotten back together and were trying to have a child. I felt lucky. I wanted to work; the future beckoned.
And yet I was so tired I could barely focus on my computer screen.
I called my doctor, a new internist. (My insurance had changed.) He did some blood work and phoned a few days later. "You're fine, just a little anemic," he said. Of course he did-for years, doctors had been telling me I was a little anemic, or a bit vitamin D deficient. He suggested that my fatigue was probably due to menstruation. Having menstruated since the age of thirteen without feeling on the verge of death, I found this explanation implausible and said as much. I could almost hear him shrug. "Try some iron supplements."
It's probably mono, a friend said. Maybe you're allergic to gluten, another suggested.
That weekend, on a crisp winter evening, I went to see a movie in the West Village with a group of friends. Afterward, as we headed for a drink, I began to feel shivery and shaky. I begged off. "Are you all right?" my friend Katie emailed the next day. "You seem run-down." I was sitting at my desk, looking at a photograph of myself as a teenager on a tall beachside dune playing with the family dog, a handsome black husky mix. A strong wind had turned my hair into streamers.
I couldn't remember when I had last felt that alive.
I went to an integrative doctor a friend recommended. She found that I had active infections of Epstein-Barr virus, cytomegalovirus (CMV), and parvovirus. She suggested some supplements and rest and sent me home. But I didn't feel better, even after the viruses appeared to resolve a month later. At the suggestion of a colleague, I called a doctor who specialized in women's health and made an appointment. In her office, as I described my symptoms and answered her unusually extensive questions about my family history-which included cancer, but also rheumatoid arthritis, ulcerative colitis, and thyroid conditions-the doctor (I'll call her Dr. E) said, "I can tell you now, before I even see your labs, I highly suspect that you have some kind of autoimmune disease."
The relief I experienced at hearing her say this was tremendous. Something was wrong: something, then, could be made right.
A few days later, she called to say that I had antibodies to my thyroid, a butterfly-shaped gland in the neck that regulates metabolism and energy. This meant my own immune system was attacking my thyroid, a disease known as "autoimmune thyroiditis," though people refer to this form of it as "Hashimoto's." Thyroiditis often results in abnormally low amounts of thyroid hormone, which leaves people sluggish and foggy.
I didn't worry about what the diagnosis meant; I was just happy to have one. Thyroid disease, I had read, is common and treatable. I knew people with it, and they were fine. The doctor told me to take a replacement thyroid hormone and check back in six weeks. By then, I would be feeling better. I sighed with relief. This was the way medicine worked in the modern world: tests told you what was wrong, and doctors told you how to fix it.
But six weeks later, I didn't feel better. I felt worse. My blood pressure was alarmingly low. I got headaches whenever I ate, and one day when I got out of bed I fainted. On another day, a burning pain shot up my neck; it felt as if someone were holding a candle to my skin. My friend Gina and I went to get a juice one afternoon-like me, she worked largely from home-and I got so dizzy that she had to steady me until I could sit. She looked at me as if I were really sick and said, "You need to try to get better, whatever that takes."
When I saw Dr. E again in late May, she didn't have much to say about my headaches and other symptoms, but she suggested raising my dosage of the hormone. I began to suspect that whatever was wrong with me wasn't going to be as clear-cut as a simple cold or a malfunctioning organ.
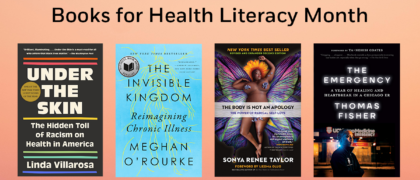
Copyright © 2022 by Meghan O'Rourke. All rights reserved. No part of this excerpt may be reproduced or reprinted without permission in writing from the publisher.